Home Care for Cracked Heels
 When the feet become too dry, the skin on the heels can harden and crack. Cracked heels can be unsightly and uncomfortable. In some cases, the cracks can be deep, painful, and may even bleed. Treating and preventing dry, cracked heels begins with establishing a daily foot care routine. Soak the feet for at least 10 minutes in plain water and pat them dry, then gently rub your heels with a loofah to remove dead skin. Next, apply a thick moisturizer to the heels and put on cotton socks to seal in the moisture. If home treatments are not effective, it is suggested that you see a podiatrist for treatment.
When the feet become too dry, the skin on the heels can harden and crack. Cracked heels can be unsightly and uncomfortable. In some cases, the cracks can be deep, painful, and may even bleed. Treating and preventing dry, cracked heels begins with establishing a daily foot care routine. Soak the feet for at least 10 minutes in plain water and pat them dry, then gently rub your heels with a loofah to remove dead skin. Next, apply a thick moisturizer to the heels and put on cotton socks to seal in the moisture. If home treatments are not effective, it is suggested that you see a podiatrist for treatment.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Foot Care Centers of Palm Beach. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our office located in Boynton Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
What Can I Do About Tarsal Tunnel Syndrome?
 Tarsal tunnel syndrome is a nerve disorder in which the posterior tibial nerve, located near the heel of the foot, is compressed. This is usually caused by participating in repetitive activities, such as running or jumping, that put stress on the nerve and surrounding areas. However, it can also be the result of a trauma, having flat feet, or being overweight. Tarsal tunnel syndrome causes foot and ankle pain, burning, tingling, and numbness. The pain usually worsens while walking and can improve with rest. There are several treatments for tarsal tunnel syndrome, including resting and icing the affected leg, taking oral pain medications, injecting steroids into the area, immobilizing the leg, wearing an orthotic, or physical therapy. In more severe cases, surgery may be needed to decompress the posterior tibial nerve. If you are experiencing the symptoms of tarsal tunnel syndrome, please seek the care of a podiatrist.
Tarsal tunnel syndrome is a nerve disorder in which the posterior tibial nerve, located near the heel of the foot, is compressed. This is usually caused by participating in repetitive activities, such as running or jumping, that put stress on the nerve and surrounding areas. However, it can also be the result of a trauma, having flat feet, or being overweight. Tarsal tunnel syndrome causes foot and ankle pain, burning, tingling, and numbness. The pain usually worsens while walking and can improve with rest. There are several treatments for tarsal tunnel syndrome, including resting and icing the affected leg, taking oral pain medications, injecting steroids into the area, immobilizing the leg, wearing an orthotic, or physical therapy. In more severe cases, surgery may be needed to decompress the posterior tibial nerve. If you are experiencing the symptoms of tarsal tunnel syndrome, please seek the care of a podiatrist.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact one of our podiatrists of Foot Care Centers of Palm Beach. Our doctors can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Boynton Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Treating Tarsal Tunnel Syndrome
Tarsal tunnel syndrome is a condition in which the tibial nerve, located in the tarsal tunnel in the foot, is compressed. The tibial nerve can become compressed from injury, such as an ankle sprain, flat feet, and lesions. Arthritis, diabetes, and varicose veins can also cause swelling and thus result in nerve compression.
Symptoms of tarsal tunnel syndrome include several different sensations in the sole of the foot, inside the ankle, and around the tibial nerve. These sensations include shooting pains, numbness or reduced sensation, pins and needles, burning, and tingling. Symptoms tend to worsen with greater activity to the area. In rare and severe occasions, this can change the muscles in the foot.
If you suspect you have tarsal tunnel syndrome, you should consult with your podiatrist. He or she will examine your medical history to see if you have a history of diabetes, arthritis, or flat feet. They will also check to see if you have suffered an injury to the area recently. An electrical test will be conducted to check if the nerve has been damaged. A simpler Tinel’s Test might also be used. This includes simply tapping the nerve to create a sensation. An MRI scan of the area may also be used.
Treatments vary greatly for tarsal tunnel syndrome. Treatments include both nonsurgical and surgical options depending upon the severity of the condition. Nonsurgical options include anti-inflammatory medication and steroid injections to the area. Orthotics, such as a splint or brace that immobilizes the foot, is another noninvasive option. For those with flat feet, custom shoes can be made to offer better foot support. Surgical options include a tunnel tarsal release, in which an incision is made behind the ankle down to the arch of the foot. This releases the ligament and relieves pressure off the nerve. Some doctors use a more minimally invasive surgery, where smaller incisions are made in the ankle and the ligament is stretched out.
If you are suffering from painful sensations in your foot, see a podiatrist who can determine if you are experiencing tarsal tunnel syndrome. Tarsal tunnel syndrome that is left unchecked can cause permanent nerve damage to the foot.
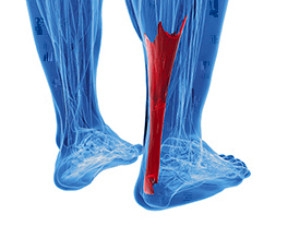
How the Achilles Tendon Can Be Injured
 The Achilles tendon is located on the back of the ankle and connects the heel to the calf muscles. The two most common injuries that affect the Achilles tendon are Achilles tendinopathy and an Achilles tendon tear or rupture. Achilles tendinopathy symptoms include swelling, stiffness, and pain that is more noticeable in the morning. An Achilles tendon tear or rupture is often the result of forceful jumping and pivoting and sudden accelerations that result in overstretching and the eventual tearing of the tendon. A complete rupture can cause severe pain and a loss of strength and movement. Because of the seriousness of an Achilles tendon injury, patients who are experiencing pain and swelling in this tendon should consult with a podiatrist. A podiatrist will be able to help provide preventative measures to avoid a rupture, as well as guide you in healing the injury.
The Achilles tendon is located on the back of the ankle and connects the heel to the calf muscles. The two most common injuries that affect the Achilles tendon are Achilles tendinopathy and an Achilles tendon tear or rupture. Achilles tendinopathy symptoms include swelling, stiffness, and pain that is more noticeable in the morning. An Achilles tendon tear or rupture is often the result of forceful jumping and pivoting and sudden accelerations that result in overstretching and the eventual tearing of the tendon. A complete rupture can cause severe pain and a loss of strength and movement. Because of the seriousness of an Achilles tendon injury, patients who are experiencing pain and swelling in this tendon should consult with a podiatrist. A podiatrist will be able to help provide preventative measures to avoid a rupture, as well as guide you in healing the injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Foot Care Centers of Palm Beach. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Boynton Beach, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
What to Do When Foot Wounds Won’t Heal
 Foot wounds, or ulcers, occur when the outer layers of the skin are damaged, thus exposing the deeper tissues of the feet. Ulcers can form due to wearing shoes that don’t fit correctly or from an injury that breaks the skin. Ulcers are most common in patients who have diabetes, neuropathy or vascular disease, and these open wounds can become infected if left untreated. While the wounds may not be painful, common signs include redness, inflammation, an odor, or thickened tissue. Patients who are at a higher risk for foot wounds, or have wounds that don’t heal, should consult with a podiatrist. Usually, a podiatrist will remove the unhealthy skin to assist with healing. Then, depending on the situation, special shoe padding, antibiotics, or surgery may be recommended for treating the wound.
Foot wounds, or ulcers, occur when the outer layers of the skin are damaged, thus exposing the deeper tissues of the feet. Ulcers can form due to wearing shoes that don’t fit correctly or from an injury that breaks the skin. Ulcers are most common in patients who have diabetes, neuropathy or vascular disease, and these open wounds can become infected if left untreated. While the wounds may not be painful, common signs include redness, inflammation, an odor, or thickened tissue. Patients who are at a higher risk for foot wounds, or have wounds that don’t heal, should consult with a podiatrist. Usually, a podiatrist will remove the unhealthy skin to assist with healing. Then, depending on the situation, special shoe padding, antibiotics, or surgery may be recommended for treating the wound.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Foot Care Centers of Palm Beach. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Boynton Beach, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.